Rebecca gave birth to Charlie at 23 weeks – the week before the legal abortion limit – and he weighed the same as a tub of butter.
A mum has spoken movingly of her shock when she realised her tiny baby – born a week before the legal abortion limit – was sharing her womb with a copper contraceptive coil, which nearly killed her and her unborn child.

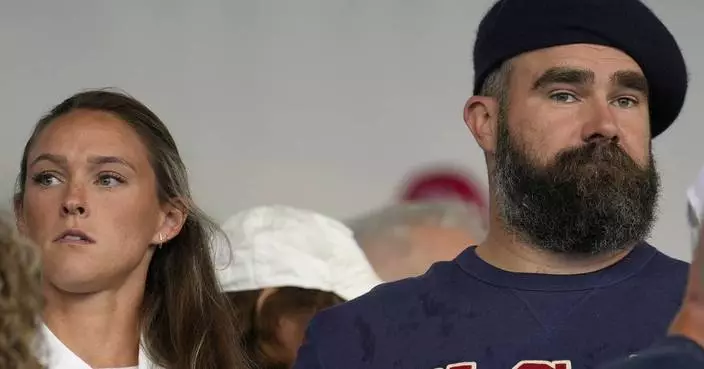
PA photo
Already a mum to Bonnie, eight, care home deputy manager Rebecca Shephard, 27, of Dagenham, Essex, recognised signs of morning sickness, despite having a 10 year copper coil, or IUD fitted – deemed 99 per cent effective.
Although she had taken steps not to fall pregnant, she and her partner, Jack Luckings, 26, who works for his family’s timber business, were both happy to have another baby.

PA photo
But things were far from straightforward, after scans showed the coil was too close to the baby in the womb for it to be removed without causing her to miscarry.
Rebecca explained: “My pregnancy was incredibly high-risk and we are so lucky that our son, Charlie, survived against the odds.
“I lost so much blood I had to have blood transfusions and we were told time and time again that I would probably miscarry.”
Not ready to have any more children, Rebecca had the IUD, which works by releasing copper, rather than hormones like other coils, into the womb, fitted after having Bonnie.

PA photo
The copper alters the cervical mucus, which makes it more difficult for sperm to reach an egg and survive and can also stop a fertilised egg from being able to implant itself.
And when she met Jack through friends in 2016, while they were happy together it was too soon for them to start trying for children.
But nature stepped in and Rebecca said: “I started to feel sick in the morning and I just knew I was pregnant. I did a test and although it was a surprise, we were really happy. We weren’t planning to have a baby at that point, as I already had Bonnie and Jack is a dad to Ava, six, but it was really exciting.
“I went to my doctor and mentioned the coil. I didn’t know anyone who’d had a coil pregnancy and wanted to know if there were any risks to the baby. My GP wasn’t sure, because it is so rare, so he recommended an early scan at seven weeks.”

PA photo
Seeing her baby for the first time, initially Rebecca was told by the sonographer that she could see no sign of the coil, so it had probably fallen out.
But just two weeks later, Rebecca started to bleed heavily for the first time.
Making her way to Queen’s Hospital, Romford, Essex, she lost so much blood that she collapsed in the hospital waiting room – coming to in a hospital bed, with Jack beside her.
“I was terrified,” she said. “I felt awful and I was so worried about the baby. They did another scan and they said that the baby was still alive, but they could see that the coil was dangerously close to him.”
She added: “At that stage, I was offered a termination, but I wanted to give the baby a chance. I wasn’t going to give up hope.”

PA photo
Rebecca was told that because of the position of the coil, close to the amniotic sac, there was a 50 per cent chance of her miscarrying and was instructed to rest.
Suffering further bouts of excessive bleeding and being rushed to hospital at 11, 15 and 17 weeks, luckily, each time, the baby was alright.
At 20 weeks, she started to bleed every day and was admitted to hospital to be monitored, where doctors discovered that a blood clot had formed around the coil, meaning she would probably suffer a late miscarriage.
Two weeks later, after a day of light bleeding, Rebecca was allowed a temporary discharge to attend Bonnie’s dance show.
But, as the performance ended, she began to bleed heavily again and this time it was mixed with some amniotic fluid.

PA photo
Rushed back to hospital, she was told her waters were leaking, but she was not in active labour.
With such serious complications, Rebecca was offered a termination again – but she refused.
Five days later, after more blood loss, she was given another blood transfusion and told the pregnancy was making her ill.
Still, she refused to abort her baby unless her life was at serious risk.
Stabilised after her transfusion, doctors began to transfer her to the more specialist neonatal intensive care unit at St George’s Hospital in Tooting, south west London.
But Rebecca went into labour as she was being transferred and, after just 23 weeks and three days in Rebecca’s womb, little Charlie was born on 17 December 2017, weighing just 1lb 4oz -the same size as a tub of butter.
He spent 116 days in hospital, battling a range of conditions including sepsis – a rare reaction to an infection, causing the body to attack itself,- and breathing difficulties.

PA photo
But, eventually, everything turned out well and in April, Rebecca and Jack were able to take Charlie home for the first time.
Rebecca said: “Bringing him home was lovely, but it was hard. He was still on oxygen but he’s such a fighter. He battled his way through all the twists and turns of his neonatal journey and is now slowly coming off oxygen. Charlie weighs 9lb 4oz and is full of fun.”
She added: “We know it might not be the end of the journey but we’re so proud of him.”

PA photo
Now, Rebecca is keen to warn other coil users of the possible dangers if they fall pregnant.
She said: “I would never use a coil again. If you have found out you are pregnant whilst on the coil, I would recommend a consultant led pregnancy and regular scans. I think more research needs to be done on IUD pregnancies.”
She continued: “There were so many different opinions among the doctors because no one really knows the best course of action at the moment.
“I was told though that not every IUD pregnancy was as complicated as mine – a lot of the time the coil can be removed or it can be positioned in a place that doesn’t have any problems.”

PA photo
Dr Diana Mansour, Vice President for Clinical Quality, Faculty of Sexual and Reproductive Healthcare (FSRH), said: “This is a rare case of a woman who made a good contraceptive choice but, unfortunately, experienced an unplanned pregnancy.”
She added: “FSRH recommends that women are informed about the very low failure rates associated with intrauterine contraception. If a pregnancy occurs with an intrauterine method in place, the device should be removed if its threads are visible.
“This will reduce the risk of infection inside the womb during that pregnancy and subsequent miscarriage or premature delivery. An ultrasound scan should also be performed to check that the pregnancy is in the womb rather than an ectopic pregnancy that can occur outside the womb.

PA photo
“Women should always talk to their GPs, practice nurses or other healthcare professionals at their local contraception and sexual health clinic if problems arise while using any method of contraception.”
For more information about how to get support after a having a premature baby, visit www.bliss.org.uk